

Hi, this is Dr. Emily Parke with your next Functional Health Minute. Today, I’m going to continue on talking about the functional medicine approach to pain. So I’m going to kind of go through next, all of the workup that we would do for someone that presents with pain as a primary concern. In my first video, we talked about pain signaling and how it works, and we briefly discussed the different types of pain. In the last video, I mentioned a little bit about the advanced blood work that we would do. Of course, we look at all the things a regular primary care doctor would look at like your blood counts, kidney and liver function, and we also look at all the hormones, adrenal, thyroid, and your sex hormones. We look at nutrient deficiencies, toxins, chronic infections, and more in just your traditional blood work. But in functional medicine, we do have access and training to look at things a little bit deeper. So we take a really deep dive into things like gut health, and there are several different tests we can do to evaluate what might be going on in the gut.
Why is that so important? Because 80% or so of your immune system is located inside your gut. If you have any type of inflammatory type of pain especially or a dysfunctional type of pain, knowing what’s going on inside the gut can really give us good insight. I did a whole series of videos in the past on all the different types of gut tests and actually all the advanced functional medicine tests, what the reports look like and what we’re testing for. So you can go back and review those. So for a functional medicine workup for pain, obviously we’re doing the advanced blood work. We’re likely going to look into the microbiome to see what’s going on. So that may be something like a stool test or a SIBO test, a part of the organic acids test gives us some information about what might be going on in the gut, but we might also look at other things like neurotransmitter markers and mitochondrial function.
We might look at other completely different things like are there food sensitivities, we’ll look at things like heavy metals, environmental toxins, mold toxins, et cetera. So there’s a lot of advanced things we can do to kind of see what we can figure out for your specific triggers because it’s different for everyone. One person with pain, it may be due to heavy metal burden. Another person, it might be nutrient deficiencies. Another person, it could be mold toxicity. Another person, it could be significant overgrowth or dysfunction or infections in the gut. So we really want to kind of tease out exactly what your specific root causes might be. So once we know what the root causes are, then of course, we’re going to put a treatment plan into place for you. Now there are some general things that are really good for pain management that will help with symptoms of any kind no matter what the cause is.
So for example, physical modalities like acupuncture or massage, physical therapy, PE and math, those that modalities can be really, really helpful to push you in the right direction and reduce your pain. But there are also some other things that I like to use in my functional medicine practice that have been quite successful and that includes something called low-dose naltrexone. I’ve written a couple of really great in-depth blogs on that medication. It is a prescription medication, it’s a compounded medication, and I am using it a lot in my auto-immune disease patients, pain management, and some really difficult to treat gut patients with really good success. It definitely helps reduce symptoms. It helps the immune system basically work better. It releases your beta=endorphins, your feel good hormones, it does a lot of things. Again, you can kind of go back and review my previous blog on that.
And then of course, we’re going to be using nutritional supplements and herbs to help with pain management. And we are going to get really specific based on the lab results with how we guide the supplements. So for example, if someone has a significant overgrowth in the gut, obviously we’re going to do a protocol that’s going to help with that. We’re going to do to get rid of the overgrowth and to heal the gut. And we’re going to replace whatever nutrients are deficient, we’re going to get things working better. But we also may prescribe some things that are not based on laboratories necessarily. For example, there’s not laboratory to tell you that curcumin might work well for you or that hemp oil might work well for you for example, but those are other kind of adjuncts and modalities that we can use to see if we can’t reduce pain and inflammation.
So curcumin and turmeric, those are like probably my top go-tos, I really love those products and there’s many different versions of those products and some work better for others just depends, you kind of have to do a trial and error there. And I have a few different recommendations that I like to use. There’s other ones though, like boswellia for example, is really good for musculoskeletal type pain. There’s ginger that can help. Magnesium is a big one, I love magnesium, especially when there’s like muscle aches and pains. Obviously magnesium can also help with other things like constipation and headaches, it’s really popular for as well. Then there’s some basic things like Omega-3 fish oil and that’s not really necessarily going to help immediately. That’s not a today, tomorrow kind of a thing. It’s more do you have a deficiency in Omega-3 fatty acids? And because the EPA part of the fish oil, there’s EPA and DHA is really anti-inflammatory long-term.
Then there’s other things that, depending on if you’ve got issues, especially with joint destruction and joint pain like MSN, glucosamine chondroitin, for example. And then there’s other modalities if you’ve got kind of auto-immune pain, if you’ve got joint pain from circulating immune complexes, then things like systemic enzymes can be really helpful there. And then of course, like I’ve mentioned many times now, like nutrient deficiency. So besides just the B vitamins, other nutrients you might not necessarily associate with a pain issue that can be significant is vitamin D for example.
I know I mentioned magnesium earlier too, but there are nutrients if they’re deficient that can be contributory to pain. So this just kind of gives you a little bit of a snippet as far as this is an example of all of a list of things that we can do in functional medicine. This is not super exhaustive, it doesn’t include every single supplement I use ever for pain, it’s the list of the common ones that I use for the different common types of pain. So again, functional medicine approach is going to be really comprehensive and look at all areas and do the best we can to figure out what your root causes are, what your triggers are for pain, so that we can get you on the healing path. This is Dr. Emily Parke with today’s Functional Health Minute.
Share:
Dr. Emily Parke
Social Media
Most Popular Posts
Subscribe To Our Newsletter
Related Posts

How Fructose Intake Affects Metabolic Health: What You Need to Know
Fructose, found naturally in fruits and added to processed foods as high fructose corn syrup, impacts health. Learn the metabolic effects of fructose intake.

Get More Vitamin D for Better Health!
Of all the vitamins and minerals you should be sure you’re getting enough of, vitamin D is perhaps one of the most important. The benefits of vitamin D are widespread and pretty incredible.

The Science Behind Protein: The Optimal Amount of Protein in the Diet Based on Age and Activity Level
Different amounts of protein are needed at different stages of life. Learn about protein, how much you need, and what happens when you don’t get enough.
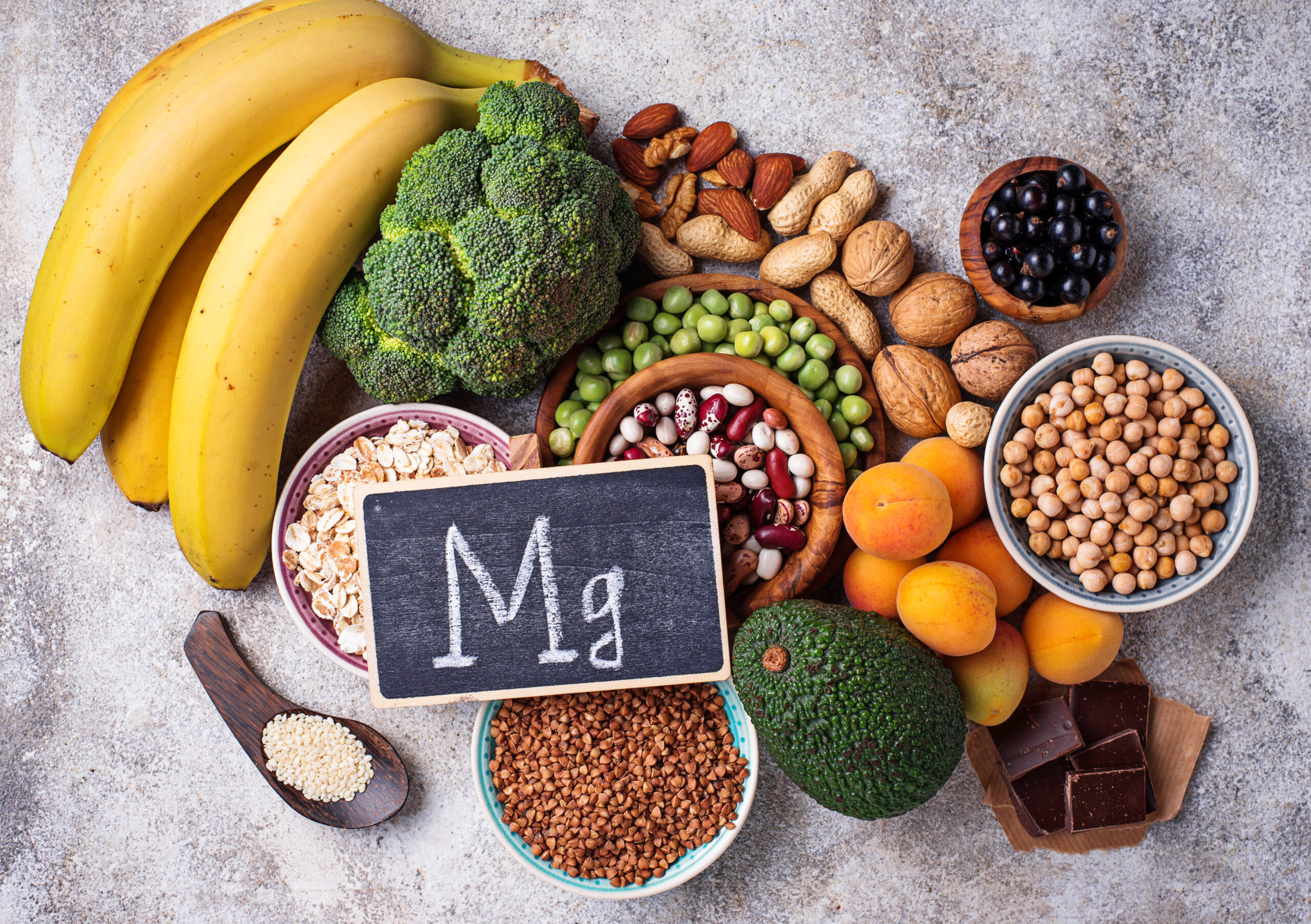
Magnesium: The Essential Mineral, Its Role in the Body, and What to Know About Magnesium Supplements
Learn about the mineral magnesium, its role in the body, how to spot magnesium deficiency, and the most bioavailable forms of magnesium to supplement with.
