
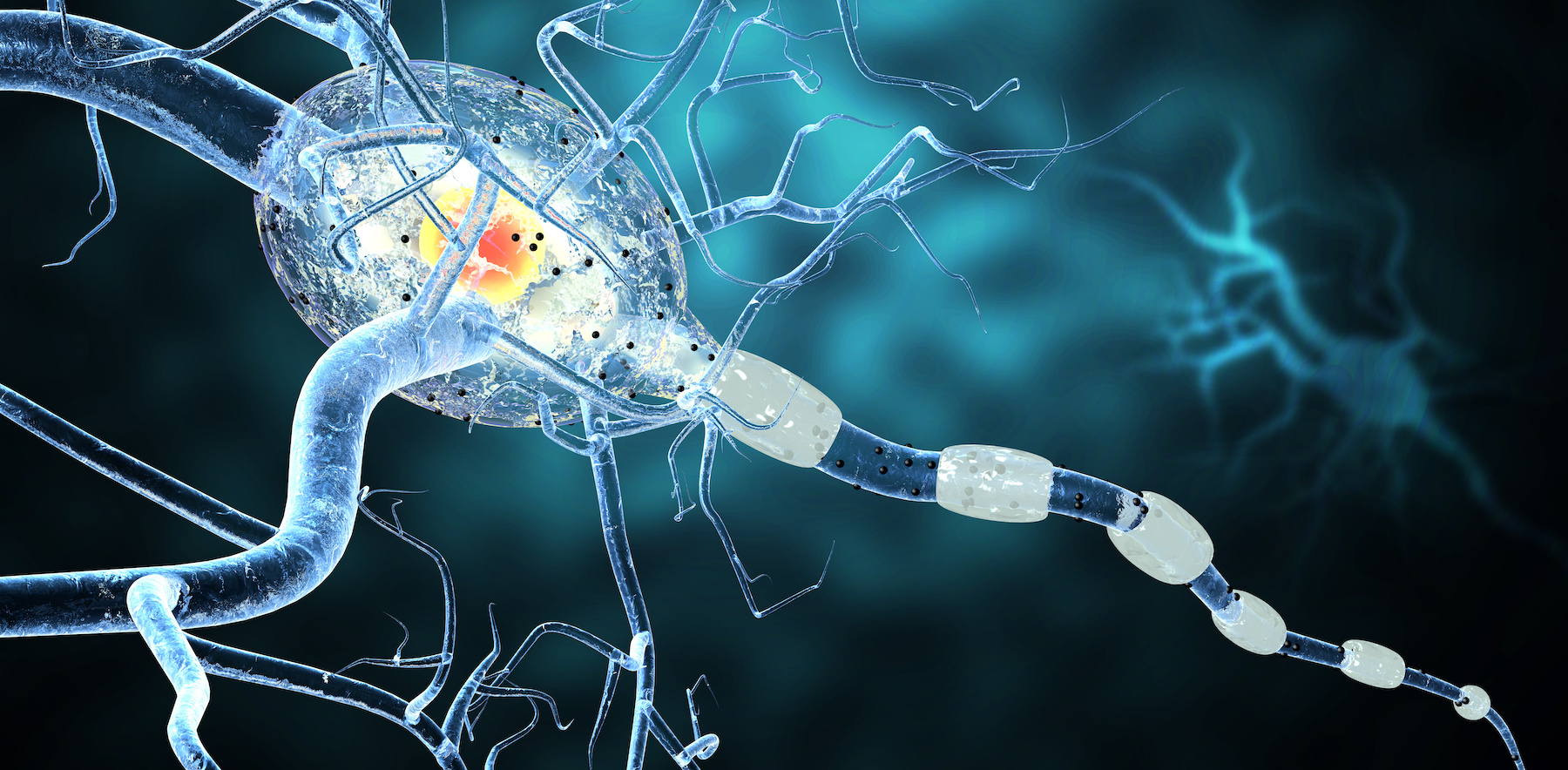
Multiple sclerosis is an autoimmune disease affecting the brain and spinal cord. It occurs when the immune system attacks the protective sheath around the nerve cells (myelin) causing nerve damage and resulting inflammation. This interferes with the communication between the brain and body, causing neurological symptoms.
It’s estimated that 2.8 million people around the world suffer from multiple sclerosis and it’s the most prevalent neurological disability worldwide. Multiple sclerosis is a progressive disease with no known cure.
Multiple Sclerosis Symptoms
Multiple sclerosis symptoms can often be hard to pin down because they vary significantly from person to person. For some, symptoms are unpredictable and inconsistent. Here are some common symptoms associated with multiple sclerosis:
- Sensory disturbances, including numbness, tingling, burning, or itching sensations.
- Lhermitte’s sign is an electric shock sensation when moving the neck in certain positions, especially when bending it forward.
- Difficulty walking due to weakness on one side of the body or in the legs and torso, tremor, lack of coordination and balance, and spasticity.
- Vision problems, including blurry vision, double vision, pain with eye movement, or loss of vision in one eye (optic neuritis)
- Fatigue
- Dizziness or vertigo
- Slurred speech
- Bladder or bowel problems
What Triggers the Onset of Multiple Sclerosis?
While there is often not a singular trigger resulting in the onset of multiple sclerosis, studies have found contributing factors that seem to play a role, including:
- Smoking
- Low levels of vitamin D
- Chronic infections such as Lyme’s disease or Epstein-Barr virus
- Genetics, although no single gene has been found responsible for the onset of multiple sclerosis
- History of obesity in the teenage years
- Being female
How is Multiple Sclerosis Diagnosed?
No single test is available to diagnose multiple sclerosis. Instead, diagnosing multiple sclerosis involves eliminating other conditions and checking for changes in the brain and spinal cord using a variety of tests and assessments.
A physical exam is one of the first things the provider will do, looking at the neurologic system, including reflexes, sensation disturbances, and strength.
Blood tests may be done to rule out other conditions, as no specific biomarker is available to determine if multiple sclerosis is present. Instead, the provider may look at several blood tests including:
- Tests to rule out infections that may cause similar neurological symptoms, such as Lyme’s disease and others.
- Antinuclear antibodies (ANA) or other immune markers to rule out other autoimmune diseases like systemic lupus erythematosus (SLE).
- A specific blood test called NMO-IgG to rule out Devic’s disease, especially for people who have symptoms of the eye from optic nerve inflammation.
- Nutrient levels such as vitamin B12 and vitamin D, since Vitamin D is a risk factor for multiple sclerosis and low levels of vitamin B12 can mimic multiple sclerosis symptoms. Other nutrient deficiencies can contribute to neurological symptoms as well.
A spinal tap can also be used as a diagnostic tool. Spinal fluid is extracted and tested for elevated levels of IgG antibodies or oligoclonal bands, whose presence can indicate multiple sclerosis.
An MRI is also usually part of the multiple sclerosis diagnostic workup, as it can show lesions of the brain or spinal cord caused by damage from multiple sclerosis.
Evoked potential tests, which measure electrical activity in the brain and spinal cord when stimulated. These tests look at how quickly information travels throughout the nervous system and can be a helpful diagnostic tool for multiple sclerosis.
Multiple Sclerosis Typical Traditional Treatments
Because there is no known cure, the goal of multiple sclerosis treatment is to shorten the duration of acute exacerbations, decrease the frequency of acute events, and provide symptom relief.
In conventional medicine, treatment often includes medications such as:
- Corticosteroids
- Beta interferons like Avonex, Betaseron, Rebif, Extavia, which are cytokines secreted by immune cells that provide antiviral and immunomodulating properties.
- Glatiramer Acetate (Copaxone), a daily subcutaneous injection that is an immunomodulator.
- Mitoxantrone (Novantrone), which was originally used to treat cancers before being FDA approved for multiple sclerosis.
- Natalizumab (Tysabri), given intravenously monthly, improves the severity of multiple sclerosis symptoms.
- Fingolimod (Gilenya), an oral medication used to prevent relapses and delay disability.
For some, a diagnosis of multiple sclerosis can come with acute exacerbations, called relapses. This is considered relapsing-remitting multiple sclerosis and is the most common form of multiple sclerosis. It consists of worsening neurological functioning, followed by times of remission.
Symptomatic care is often focused on during times of relapses, targeting symptoms like fatigue, pain, stiffness, and bladder dysfunction. Two medications that can help treat acute relapse and speed up recovery include corticosteroids like methylprednisolone and prednisone, both of which are also anti-inflammatory.
Other lesser used treatments include stem cell therapy, which is being proposed as a potential treatment for multiple sclerosis patients.
The Functional Medicine Approach to Multiple Sclerosis Treatment
Functional medicine takes a well-rounded, holistic approach to multiple sclerosis treatment. While medications may still be used, additional treatment options are often done concurrently, including physical, speech, and occupational therapies; a balance of exercise and rest; stress management, toxin reduction and a whole foods anti-inflammatory diet. In combination with more traditional medications, these functional medicine multiple sclerosis treatment approaches support symptom relief and improve quality of life.
Nutrition For Multiple Sclerosis
Eating a whole-foods, anti-inflammatory diet with a paleo focus can support symptom relief. Here are some tips:
- Avoid processed foods, gluten, and dairy. A study completed in over 25 countries showed that cow’s milk is associated with a higher incidence of multiple sclerosis.
- Increase fresh fruits and vegetables, focusing on sulfur rich foods like those in the brassica family, mushrooms, and onions to support nerve cell function, improve detoxification pathways, and increase neuroprotection.
- Eat more dark leafy green vegetables and deeply pigmented foods like blueberries for neuroprotection.
- Consider adding in organ meat, grass fed meat, and wild caught fish.
- Eat more fermented foods like kimchi and fermented vegetables to support the gut microbiome.
For more detailed information on this specific form of a Paleo food plan for Multiple Sclerosis that has been researched visit https://terrywahls.com/. Dr. Wahls is doing current MS research and has reversed her own MS using a Paleo approach combined with Functional Medicine.
As with other autoimmune diseases, doing advanced testing to look at inflammation levels, gut health, toxin load, infections and nutrient deficiencies is also important.
Vitamin and Mineral Supplementation for Multiple Sclerosis
Both vitamin D and omega-3 fatty acid supplementation have been studied in relation to multiple sclerosis. While additional studies are needed to further understand the connection, supplementing with both vitamin D and omega-3 fatty acids support overall brain function. However, checking for and treating other nutrient deficiencies are important, as the goal is to have a well functioning immune system. For example, zinc is another crucial immune system nutrient and lower levels have been found in autoimmune disease patients. There are MANY other nutrients that play a role in properly functioning immune and nervous systems as well (like certain B vitamins for example).
Low Dose Naltrexone
LDN a compounded prescription medication that has been shown to act as an anti-inflammatory agent in the central nervous system, through the microglial cells – in both opioid and non-opioid receptors. It’s through these pathways that low dose Naltrexone is believed to be effective in reducing pain and inflammation in a number of autoimmune diseases.
The microglia are cells located in the central nervous system and are considered part of immune system cells. These cells often become activated by triggers, which causes inflammation throughout the body. Low dose Naltrexone has an antagonistic effect on these cells, which calms the overreaction of the immune system down. Thus, reducing inflammation and pain throughout the body.
A Functional Medicine Approach to Multiple Sclerosis Treatment
Struggling with inconsistent neurological symptoms and aren’t sure what to do? Functional medicine can help. A proper functional medicine approach takes a holistic, whole-body approach to get to the source of your symptoms and find the best treatment for you. By viewing health as multidimensional, functional medicine allows for a well-rounded picture of your health history by looking at current symptoms, diet, psychological health, and past treatments.
At Arizona Wellness Medicine, our team of highly trained functional medicine providers can offer this. With a complete picture of your health history, your current symptoms, your diet, and more, we can get to the bottom of your neurological symptoms to make a personalized treatment plan that works for you. Discover how Arizona Wellness Medicine can help here.
Resources:
- Multiple Sclerosis and Autoimmunity: A Veiled Relationship
- Multiple Sclerosis: Pathogenesis, Symptoms, Diagnoses and Cell-Based Therapy
- Lhermitte Sign
- Multiple Sclerosis Review
- The Many Faces of Cobalamin (Vitamin B12) Deficiency
- The value of oligoclonal bands in the multiple sclerosis diagnostic criteria
- Assessment of lesions on magnetic resonance imaging in multiple sclerosis: practical guidelines
- A new role for evoked potentials in MS? Repurposing evoked potentials as biomarkers for clinical trials in MS
- Treatment of Acute Relapses in Multiple Sclerosis
- Dietary Approaches to Treating Multiple Sclerosis-Related Fatigue with Terry Wahls, MD
Share:
Dr. Emily Parke
Social Media
Most Popular Posts
Subscribe To Our Newsletter
Related Posts

How Fructose Intake Affects Metabolic Health: What You Need to Know
Fructose, found naturally in fruits and added to processed foods as high fructose corn syrup, impacts health. Learn the metabolic effects of fructose intake.

Get More Vitamin D for Better Health!
Of all the vitamins and minerals you should be sure you’re getting enough of, vitamin D is perhaps one of the most important. The benefits of vitamin D are widespread and pretty incredible.

The Science Behind Protein: The Optimal Amount of Protein in the Diet Based on Age and Activity Level
Different amounts of protein are needed at different stages of life. Learn about protein, how much you need, and what happens when you don’t get enough.
Magnesium: The Essential Mineral, Its Role in the Body, and What to Know About Magnesium Supplements
Learn about the mineral magnesium, its role in the body, how to spot magnesium deficiency, and the most bioavailable forms of magnesium to supplement with.
