

Graves’ disease, an autoimmune disease of the thyroid gland, was originally described by and named after physician Robert James Graves in 1835. It causes hyperfunction of the thyroid gland, leading to an enlarged thyroid, and is believed to be caused by antigen-antibody reactions in the thyroid. Around 60-80% of all hyperthyroidism cases are due to Graves’ disease
Graves’ Disease Symptoms
The three main symptoms of Graves’ disease include goiter (an enlarged thyroid or extra thyroid tissue from a mass or irregular cell growth); an eye condition called Graves’ ophthalmopathy that causes bulging eyes, redness, grittiness in the eyes, and retracting of the upper eyelids; and hyperthyroidism or thyrotoxicosis symptoms including:
- Irregular heartbeat (arrhythmia)
- High heart rate (tachycardia)
- Heart palpitations
- Unexplained weight loss
- Muscle weakness
- Overactive reflexes
- Anxiety or irritability
- Fatigue
- Insomnia
- Heat intolerance and increased sweating
- Tremors, often in the hands
- Increased appetite
- More frequent bowel movements
- Changes in menstrual cycle
Graves’ dermopathy can also occur, which is a thick red layer of skin found on the top of the feet or shins. It’s considered one of the more uncommon extrathyroidal manifestations, often occurring with ophthalmopathy.
While Graves’ disease is commonly thought of as only affecting the thyroid tissue, it actually is part of a more extensive autoimmune thyroid disease (AITD), which can lead to the dysfunction of other organs as well.
What Happens When Graves’ Disease is Severe?
When left untreated, Graves’ disease symptoms can cause a variety of unwanted and potentially life altering issues, including loss of sight, serious issues during pregnancy, and heart disorders such as atrial fibrillation. It also has the potential to cause a severe condition called thyroid storm. This is an acute emergency and medical intervention is needed right away. Thyroid storm symptoms include:
- High temperature
- High heart rate, or tachycardia
- Hand tremors
- Overactive reflexes
- Swelling and bulging of the eyes
- Jaundice
- Systolic hypertension, when the top number of the blood pressure reading is above 140 (normal is 120/80)
While many of the symptoms of thyroid storm can mimic symptoms of Graves’ disease, the difference lies in their severity and the fast onset of multi-body symptoms. Diagnosis of thyroid storm is made through a provider’s clinical observation and full body decompensation with a known precipitating factor or trigger, such as an illness. The mortality rate of thyroid storms is high, up to 25%, despite advanced medical interventions, so it’s treated as a life-threatening emergency. If you or your provider has an early suspicion of this, a prompt diagnosis and intensive medical management is needed.
Graves’ Disease Risk Factors
Risk factors for developing Graves’ disease include:
- Being under the age of forty
- Female
- Presence of another autoimmune disease
- Family history of Graves’ disease
- Being a smoker
- Pregnant or postpartum
How is Graves’ Disease Diagnosed?
There are a variety of diagnostic tools your functional medicine provider may use to diagnose Graves’ disease, including a blood test, radioactive iodine update (RAIU), imaging, and a physical exam.
Blood Tests for Graves’ Disease
Three blood tests can be helpful in the diagnosis of Graves’ disease: TSH, thyroid hormones T3 and T4, as well as TRAb and TSI.
- TSH, or thyroid stimulating hormone, is lower than normal with Graves’ disease. This is because the brain detects higher levels of T3 and T4 and doesn’t want to make more TSH.
- Thyroid hormones T3 and T4 are both very high in Graves’ disease, so your provider will often check these when thyroid concerns are present. We look at both total and free levels as well as the reverse T3.
- TRAb is an antibody that triggers the release of thyroid hormones T3 and T4. TRAb is considered a gold standard in diagnostic testing for Graves’ disease, as it helps reduce the number of incorrect diagnoses based on clinical symptoms. High levels of TRAb indicate Graves’ disease, but if lab results don’t show high amounts, another type of hyperthyroidism may be present.
Radioactive Iodine Uptake (RAIU)
Iodine is crucial to thyroid function, helping the gland make both T3 and T4. With a radioactive iodine uptake test, a small amount of radioactive iodine is ingested. The provider then uses a probe to measure the rate of iodine absorption in the thyroid, helping to diagnose thyroid dysfunction.
Imaging Tests for Graves’ Disease
An ultrasound is an imaging test often used as an alternative to RAIU, especially in pregnant women who can’t be exposed to radiation. The ultrasound can identify an enlarged thyroid and the presence of nodules, masses, or cysts.
Physical Exam for Graves’ Disease
After a thorough discussion of symptoms, your functional medicine provider will complete a physical exam, looking for signs of Graves’ disease. This often includes an examination of the eyes, skin, and checking for goiter in the neck.
Graves’ Disease Treatment: Graves’ Disease Medications
After getting diagnosed, a range of Graves’ disease treatment options can be used depending on the severity of the disease. Common treatment options include targeted Graves’ disease medications to suppress overactive thyroid function including:
- Glucocorticoid steroids: These medications reduce the conversion of T4 to T3, helping lower thyroid hormone in the body. However, long-term glucocorticoid steroid use leads to more harm than benefits and is not always considered a first line of treatment.
- Anti-thyroid medications like propylthiouracil (PTU) or methimazole, which interfere with iodine metabolism in the thyroid gland.
Other Graves’ disease treatment options include beta blocker medications for cardiac symptoms, radioactive iodine therapy, and surgery to remove most or all the thyroid gland. Treatment can also be targeted towards eye symptoms from Graves’ ophthalmopathy using steroids, orbital decompression surgery, or specialized glasses to correct double vision.
While treatment can be successful, relapse is common in the course of Graves’ disease treatment. But, certain lifestyle changes may prevent relapse, including diet changes, stopping smoking and optimizing nutrient deficiencies (like vitamin D3 and selenium).
Lifestyle Changes for Graves’ Disease
Lifestyle changes that can slow the progression of Graves’ disease include exercise, eating a paleo diet, and reducing stress and toxin exposure.
Exercise For Graves’ Disease
Structured exercise, consisting of daily walking, stretching, and strengthening exercises, has a significant impact on normalizing the thyroid profile in patients with Graves’ disease. Exercise also improves aerobic capacity and helps reduce fatigue, often a significant symptom for those with Graves’ disease. Another benefit of exercise can include a reduction in the need for thyroid medication long-term.
Starting an exercise program is a great lifestyle choice to not only support healthy thyroid function, but also overall health. Start with daily walking, even if it’s just for 5 minutes, and work up to 30 minutes a day, 5 days a week. Adding in stretching and strengthening exercises can also help normalize thyroid function according to this study.
Paleo Diet and Graves’ Disease
Interestingly, those with Graves’ disease often also have gluten intolerance – providing a link between thyroid function and gut health. This makes a healthy diet all the more important for managing Graves’ disease.
A general guideline to start with is to focus on anti-inflammatory, whole foods – often what you find in the paleo diet. Avoid any grains with gluten, processed sugars, and dairy. Instead focus on what our ancestors ate – fresh fruits, vegetables, nuts, seeds, and lean meats as tolerated.
Stress Management for Graves’ Disease
According to one study looking at stress and the onset of Graves’ disease, researchers found that stress is an important factor in the onset of Graves’ disease. Previous studies have even linked the occurrence of anxiety and depression with Graves’ disease, making stress reduction and coping skills an important part of functional medicine treatment of the disease.
Finding ways to reduce and manage stress is an important, but often overlooked part of treatment. There are so many resources out there to help with managing stress. Here are a few on meditation and ways to combat stress, Many stress management techniques include eating a balanced diet, incorporating movement into your daily routine, finding ways to be mindful, and getting quality sleep.
Reduce Toxin Exposure
Environmental toxins play a role in thyroid dysfunction. These toxins can interfere with many aspects of thyroid function including hormone synthesis, hormone metabolism, hormone excretion, and hormone action. Reducing environmental toxin exposure is important to minimize any impacts of these toxins on thyroid health.
Here are some tips to start with:
- Choose organic foods whenever possible (especially avoid the dirty dozen).
- Filter your water using a reverse osmosis water filtration system before drinking, as contaminants can be rampant in drinking water.
- Consider using an air filter inside your home (two great brands are IQAir and Austin Air).
Looking for more resources on environmental toxins? Here’s how to detoxify from environmental exposures and how to reduce toxin exposure.
Arizona Wellness Medicine and A Functional Medicine Approach to Graves’ Disease Treatment
Graves’ disease and other thyroid conditions can be frustrating, especially when you’re still working to diagnose the issue. But functional medicine offers a unique approach to target your whole-body symptoms and find relief.
As a functional medicine clinic, our providers at Arizona Wellness Medicine look at your whole health picture, taking a comprehensive history, looking at your Graves’ disease symptoms, completing a physical assessment, ordering diagnostic studies as needed, and coming up with a personalized Graves’ disease treatment plan that works for you. We are dedicated to getting to the bottom of your symptoms to help you find lasting relief. Discover how our functional medicine approach to treatment at Arizona Wellness Medicine can help here.
Resources:
- Current Diagnosis and Management of Graves’ Disease
- Graves’ Disease Mechanisms: The Role of Stimulating, Blocking, and Cleavage Region TSH Receptor Antibodies
- Dermopathy of Graves’ disease: Clinico-pathological correlation
- Graves’ Ophthalmopathy
- Thyroid Storm
- Reproducibility of radioactive iodine uptake (RAIU) measurements
- Diagnosis and management of Graves’ disease
- Clinical diagnosis of Graves’ or non-Graves’ hyperthyroidism compared to TSH receptor antibody test
- Current and Future Treatments for Graves’ Disease and Graves’ Ophthalmopathy
- Structured exercise program improves functional capacity and delays relapse in euthyroid patients with Graves’ disease
- What is the impact of stress on the onset and antithyroid drug therapy in patients with graves’ disease: a systematic review and meta-analysis
- Environmental Exposures and Autoimmune Thyroid Disease
Share:
Dr. Emily Parke
Social Media
Most Popular Posts
Subscribe To Our Newsletter
Related Posts

How Fructose Intake Affects Metabolic Health: What You Need to Know
Fructose, found naturally in fruits and added to processed foods as high fructose corn syrup, impacts health. Learn the metabolic effects of fructose intake.

Get More Vitamin D for Better Health!
Of all the vitamins and minerals you should be sure you’re getting enough of, vitamin D is perhaps one of the most important. The benefits of vitamin D are widespread and pretty incredible.

The Science Behind Protein: The Optimal Amount of Protein in the Diet Based on Age and Activity Level
Different amounts of protein are needed at different stages of life. Learn about protein, how much you need, and what happens when you don’t get enough.
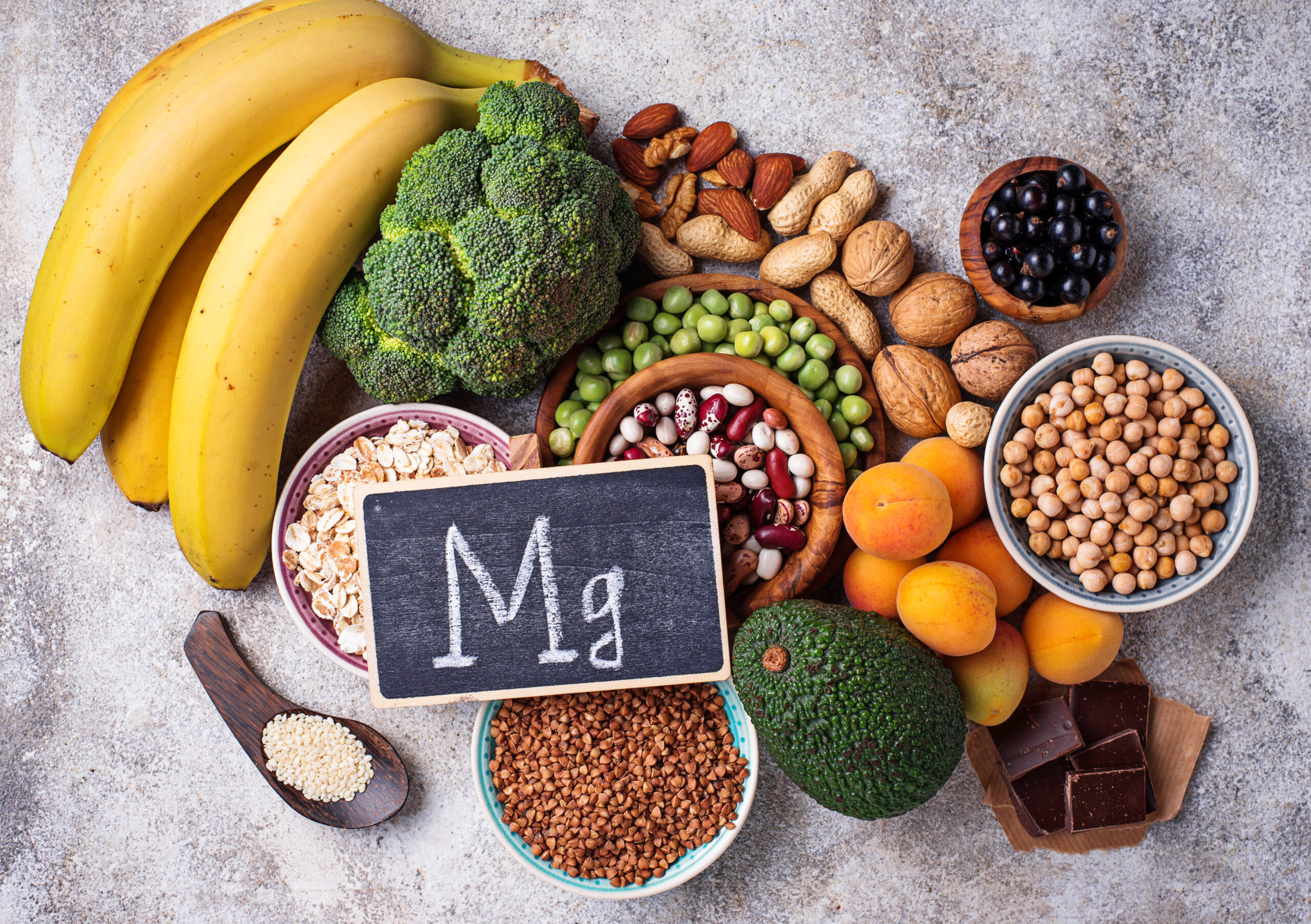
Magnesium: The Essential Mineral, Its Role in the Body, and What to Know About Magnesium Supplements
Learn about the mineral magnesium, its role in the body, how to spot magnesium deficiency, and the most bioavailable forms of magnesium to supplement with.
