

On top of everything else, you now have blurry vision, eye pain, and difficulty focusing. If only autoimmune disease and inflammation could stick to one part of your body!
If you’re currently experiencing any of these symptoms, or there’s been a sudden change to the health of your eyes, you must seek medical care as a matter of urgency. Never risk your eyes – with many ocular diseases, seeking treatment as soon as possible offers the best outcome.
You might have only just discovered that inflammation can affect your eyes, or you may be used to regular uveitis flare-ups. Inflammation is such a cornerstone of chronic disease – but what happens when your eyes are affected?
What Is Uveitis?
Uveitis is a form of inflammation in the eye that affects the uvea. It comes on suddenly and worsens quickly, and it’s important to seek out treatment as soon as possible.
Your uvea is made up of the:
- Iris – the colored circle that controls the amount of light that enters your eye.
- Ciliary body – responsible for creating the aqueous humour within the eye and controlling the shape of your lens and size of your pupils.
- Choroid – the vascular and connective tissue layer of the eye, sitting between the retina and the sclera (the white of the eye).
Iritis (anterior uveitis) is the most commonly found subtype of uveitis, and it affects the iris. Intermediate uveitis attacks the ciliary body, and choroiditis and retinitis (posterior uveitis) affect the choroid and the retina. When all sections of the uvea are inflamed, it’s called diffuse uveitis.
Uveitis symptoms include:
- Redness of the eye
- Eye pain
- Photophobia (sensitivity to light)
- Increased number of floaters in your vision
- Blurred vision
- A sudden worsening of sight
The inflammation behind uveitis can be caused by injury, infection – or an autoimmune disease. If you experience any sudden pain in your eye, or the symptoms above, you should seek care as soon as possible.
What Causes Recurrent Uveitis?
Recurrent uveitis can be frustrating – it seems to flare up with no warning. Sometimes the disease can be chronic – particularly if it’s intermediate or posterior uveitis. And although the inflammation is contained in the eye, it can be triggered by an irregular immune response elsewhere in the body.
Uveitis is linked with the following autoimmune and infectious diseases:
- Lyme disease – The anterior form is seen frequently in patients with Lyme disease, and a wide variety of eye inflammation can occur in the early stages of the disease.
- Crohn’s disease and ulcerative colitis – Flares of uveitis may sync with symptoms of Crohn’s disease, but there is no direct link between the activity of uveitis and ulcerative colitis.
- Sarcoidosis – The ocular form of sarcoidosis causes uveitis – alongside other eye diseases.
- Ankylosing spondylitis, including psoriatic arthritis – The HLA B27 antibody is typically high in patients with this type of disease. Half of all patients with anterior uveitis have high levels too. Anterior uveitis may be considered as an early sign of ankylosing spondylitis in future.
- Behcet’s disease.
Uveitis needs to be managed, as if left untreated it can progress into a permanent loss of sight. That said, many patients reduce their chances of it recurring by finding a way to manage underlying inflammation.
What is Behcet’s disease?
Behcet’s disease is a tricky autoimmune disease of the blood vessels that causes several symptoms that may seem unrelated at first. As it can affect a wide variety of arteries and veins in a variety of sizes, it has a wide-ranging effect on your body.
Behcet’s disease symptoms may include:
- Painful mouth sores that resemble cankers.
- Genital sores – painful, red open sores on the vulva or scrotum.
- Acne sores or raised nodules on the skin.
- Swelling and pain in joints – especially your knees.
- Uveitis – see above. As the uvea contains the vascular layer, Behcet’s disease can quickly cause complications in the eye, including red looking eyes, blurry vision, and pain.
- Swelling that may be caused by blood clots.
- Abdominal pain, diarrhea, or bleeding when passing stools.
- Fever and disorientation.
- Poor balance or headache.
If these symptoms seem familiar, it’s crucial you seek diagnosis right away, as Behcet’s disease can cause a number of serious complications, including increased for blood clots and stroke.
How Is Behcet’s Disease Diagnosed?
Behcet’s disease can be a challenge to diagnose, but your doctor can use a range of exams and tests to rule out other diseases. These include:
- Physical exam – to examine mouth and genital sores, abnormal skin changes, or swelling.
- Blood tests and urine tests – mostly to rule out other autoimmune diseases, as there is not one specific diagnostic test for it.
- Imaging exams – can help rule out other conditions, and also check for damage to organs.
- Skin biopsy – to check for antibodies associated with Behcet’s disease.
- Pathergy test – a skin prick test that checks for the hypersensitivity typical of Behcet’s disease.
Finally, your doctor may be able to diagnose Behcet’s disease if you’ve had at least three episodes of mouth ulcers over the 12 weeks, and two of the following symptoms: eye inflammation, hypersensitive skin, skin lesions, or genital ulcers.
What Are the Symptoms of Optic Neuritis?
Optic neuritis is an inflammatory eye disease characterised by temporary vision loss.
Optic neuritis symptoms include:
- Mild to severe loss of vision in one eye, which can last from a week to 10 days
- Pain around your eye that feels worse when you move the eye
- Poor perception of colors
- Changes in the way your pupil moves in bright light
- Photopsia – where you can see flashing lights at the edge of your vision
- Vision worsening when your body temperature increases
Optic neuritis needs to be diagnosed and treated, as any changes to vision or the feel of your eye should always be checked out.
What Causes Optic Neuritis?
Optic neuritis occurs when the optic nerve that connects the eye with the brain becomes inflamed. The optic nerve carries the visual information to your brain, so the symptoms reflect the interruption of this crucial service – loss of vision, and lack of feedback from the brain to manage the response to light.
Most cases of the disease have no apparent cause. But optic neuritis has been linked with the following diseases:
- Multiple sclerosis – optic neuritis can be an early warning sign of MS
- Lyme disease – rarely reported, but there is a link
- Sarcoidosis
- Guillain-Barre syndrome – occurs in rare cases
- Systemic lupus erythematosus
- Behcet’s disease
If you have optic neuritis alongside another inflammatory disease, it may be time to start treating your body as a whole, and work on reducing underlying inflammation.
How Can Functional Medicine Help With Autoimmune Diseases of the Eye?
Conditions such as optic neuritis and uveitis can occur out of nowhere – but they can also be an indication of underlying inflammation or a complication from an autoimmune disease. If you have recurrent uveitis or a sudden attack of optic neuritis, it can be very frustrating and upsetting to deal with the pain – especially on top of another condition.
Functional medicine practitioners do extensive testing to look for the root causes and spend time with you to hear all of your concerns. We’re not interested in surface treatments: we want to help you tackle the underlying issue – in this case, inflammation – that is causing your symptoms to flare up. We look at your entire health – your health history, your diet, current levels of stress, sleep quality, exercise and movement and toxin exposures. Also, in any autoimmune disease, the gut is of utmost importance, thus there is a big focus on gut testing and gut healing as well.
If you’re looking to reduce your inflammation and autoimmune disease symptoms in the Phoenix, Scottsdale, Paradise Valley, Arizona area, call to book an appointment at 602 892-4727 or fill out our contact form. If you’re not local to us, try out my 7 Weeks to Your Healthiest Self – this masterclass that provides you with the benefits of functional medicine – from the comfort and privacy of your own home.
Share:
Social Media
Most Popular Posts
Subscribe To Our Newsletter
Related Posts

How Fructose Intake Affects Metabolic Health: What You Need to Know
Fructose, found naturally in fruits and added to processed foods as high fructose corn syrup, impacts health. Learn the metabolic effects of fructose intake.

Get More Vitamin D for Better Health!
Of all the vitamins and minerals you should be sure you’re getting enough of, vitamin D is perhaps one of the most important. The benefits of vitamin D are widespread and pretty incredible.

The Science Behind Protein: The Optimal Amount of Protein in the Diet Based on Age and Activity Level
Different amounts of protein are needed at different stages of life. Learn about protein, how much you need, and what happens when you don’t get enough.
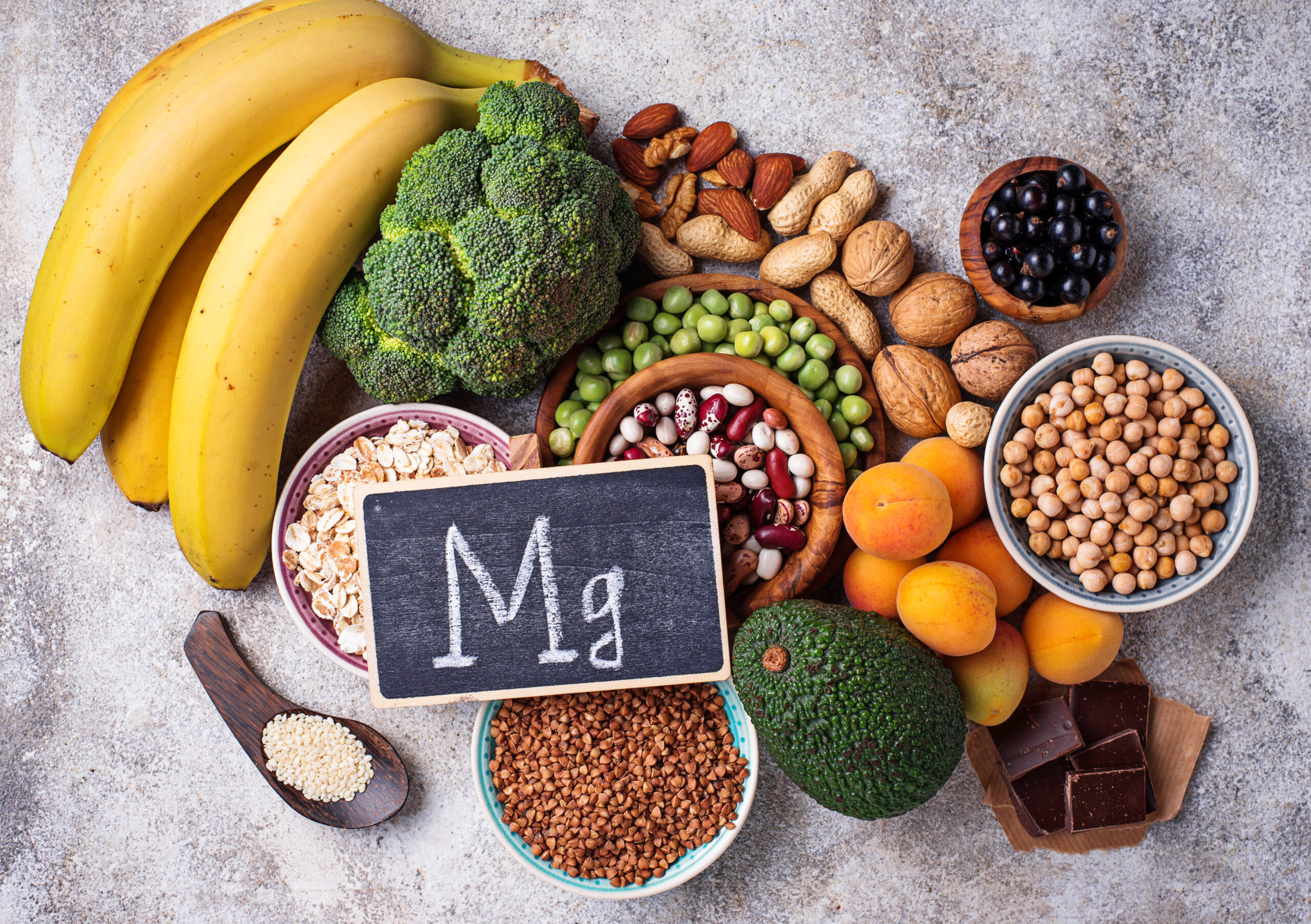
Magnesium: The Essential Mineral, Its Role in the Body, and What to Know About Magnesium Supplements
Learn about the mineral magnesium, its role in the body, how to spot magnesium deficiency, and the most bioavailable forms of magnesium to supplement with.
